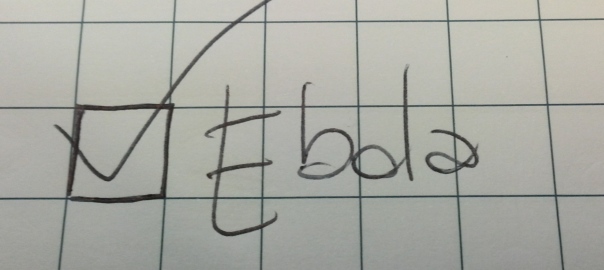
A man goes to the hospital saying he is not feeling very well. Medical staff, due to the international health alarming situation is trained to fill a pre-assessment checklist in which information about recent travel itineraries has to be reported. The man says to the nurse he has just come back from a journey in West Africa, in particular from Liberia. A tick is placed in the provided box. However, that information is not fully communicated to the doctor who, after a diagnosis of low-grade fever from a viral infection, sends the patient home with antibiotics. After three days the man is hospitalized in the isolation room with a completely different diagnosis: Ebola.
This happened between 24 and 28 September in Dallas, Texas. The press conference held by the Centre of Disease Control and Prevention Director Dr. Tom Frieden, rightly addresses relevant aspects to contain possible panic of contamination of the USA public: no risk for those who were flying with Mr. Duncan (the Ebola infected man) as at that time he had not symptoms of the illness and so he could not infect other people; the contacts-track-system is in place to find and monitor all those who have had contact with Mr. Duncan during his staying in the USA since the symptoms appeared and before he has been hospitalized.
Dr. Tom Frieden press conferenceApparently there are no serious reasons for warring about the fact that this infection can turn into the American hotspot for the pandemic and cases abroad, especially in US and UK, were estimated to be by the end of September [1].
That said, what is alarming is the inefficiency of the information and communication management in relation to the case. The checklist-approach to collect relevant data is undoubtedly efficient as it contributes to focus the gathering process only on specific domains and to reduce rooms for their free interpretation but, as it has already been proved in other cases particularly within the healthcare system, it cannot be a left alone instrument.
The failure highlights a fundamental aspect of the crisis management: the role of communication. Communication in emergency can be considered as a highly complex and tightly coupled system. Adapting what is known about technical systems [2] to communication, its complexity is given by the limited possibility of isolating failed parts, the numbers of different perspectives from which it can be addressed that do not represent the complexity of the system itself, the sometimes limited awareness of all the actors involved in it about their interdependencies together with possible misinterpretation of its contents. On the other side, communication in emergency follows a sort of invariant sequence of steps, it has limited potential for substitution and in some cases lacks of redundancy. Redundancy is a sort of assurance for crisis managers that other “backup systems” are in place in order to reduce the possibility of malfunctioning of alarming primary resources.
The use of a checklists alone has to be handled with care since they do not easily provide this possibility. As a matter of fact information on the Texas Health Presbyterian Hospital checklist did not go completely through resulting in, I would say serious, failure of the system. Other solutions that are able to comprehend this tool into a more “virtuous” circle, providing a more conscious, shared and focused communication process has not to be newly invented as they already exist. Thus, what is left is simply the “regret” of Mark C. Lester, executive vice president of the Hospital that this failure happened [3] and the nth lesson-to-be-learnt which hardly seems easy to be learnt.
[1] http://news.sciencemag.org/health/2014/08/disease-modelers-project-rapidly-rising-toll-ebola
[2] Perrow, C. 1984. Normal accidents: living with high-risk technologies. Princeton: Princeton University Press
[3] http://guardianlv.com/2014/10/ebola-dallas-hospital-ignored-alarm-bells/